Staphylococcus aureus is a bacterium commonly found in the noses of about 30% of individuals and on the skin.
Most of them are not harmful but sometimes it can cause infections. In hospital settings, these infections can lead to fatal or serious infections. Also, some S. aurei are resistant to common antibiotics.
Taxonomy and Classification
KINGDOM: Bacteria
PHYLUM: Firmicutes
CLASS: Bacilli
ORDER: Bacillales
FAMILY: Staphylococcaceae
GENUS: Staphylococcus
SPECIES: aureus
Morphology and Microscopy
- Gram positive cocci, singly, in pairs or in a short chain of 3-4 bacteria.
- Catalase positive and oxidase negative with exception of S. sciuri group.
- Approximately 0.5-1.5 µm in diameter.
- Non motile, Non-sporing and Non-flagellated
- Facultative anaerobes (except S. aureus anaerobious).
- Clusters (grape –like) arrangement.
- Capsulated
- Many strain produce staphylococcal enterotoxins, exfoliative toxins and the superantigen toxic shock syndrome toxin.
Under microscope, they are seen as purple grape like clusters. They may also occurs in pairs or in shorts chains. These clusters help to distinguish staphylococcus from streptococcus.
Cultural and Growth Characteristics
- Grow on most media under both aerobic and microaerophilic conditions.
- Optimum temperature: 37˚C
- Optimum pH : 7.4-7.6
- Aerobes and facultative anaerobes
- On solid media colonies are smooth, round, glistening and raised.
- Usually forms grey to deep golden yellow colonies.
- Mac Conkey Agar: Lactose fermenting pink colonies.
- Mannitol Salt Agar: 2-3mm, circular, smooth, shiny surface, opaque and golden yellow colonies.
- Blood Agar: shows β-hemolysis.
- Brain Heart Infusion Agar: yellow pigmented colonies
- Tryptic Soy Agar: convex, circular and entire margin colonies.
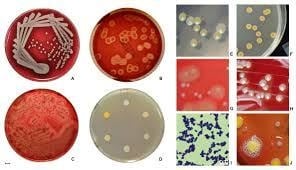
Figure: Growth of S. aureus on different media
Source: Medical Laboratory Scientist (MLS) https://medicallabscientist.org/staphylococcus-aureus-cultural-characteristics/
Biochemical and Identification tests
| Tests | Properties |
| Gram Staining | Positive |
| Catalase | Positive |
| Oxidase | Negative except S. sciuri group |
| Indole | Negative |
| MR (Methyl Red) | Positive |
| VP (Voges Proskauer) | Positive |
| Citrate | Positive |
| H2S | Negative |
| Motility | Negative |
| Capsule | Non-capsulated |
| Gas | Negative |
| Gelatin Hydrolysis | Positive |
| Coagulase | Positive |
| Hemolysis | Positive |
| Fermentation of | |
| Glucose | Positive |
| Fructose | Positive |
| Galactose | Positive |
| Lactose | Positive |
| Mannitol | Positive |
| DNase | Positive |
| Arabinose | Negative |
| Cellobiose | Negative |
| Sucrose | Positive |
| Enzymatic Reactions | |
| Acetoin Production | Positive |
| Alkaline Phosphatase | Positive |
| Arginine Dehydrolase | Positive |
| Hyaluronidase | Positive |
| Lipase | Positive |
| Ornithine Decarboxylase | Negative |
Pathogenesis and Virulence Factors
- Approximately 30-50% of adult anterior nares carry S. aureus which remain dormant without causing infections for weeks to months.
- The colonization of organisms begin infection under certain factors like immune suppression, surgeries, prolonged hospitalization, use of invasive medical devices or chronic metabolic diseases.
- Localized skin abscess proceeds after the inoculation of organisms in skin.
- Then the organisms enter into blood stream and spread to different parts of body resulting in sepsis.
- This spread can result in osteomyelitis, renal carbuncle, endocarditis, septic arthritis. Other clinical infections include meningitis, toxic shock syndrome and UTI.
S. aureus posses various virulence factors which enable organisms to cause wide range of infections in both humans and animals. These factors helps in various steps like attachment of pathogen to host cells, break down the host immune shield, invasion of tissues and so on. Based on their mechanism of action, these factors are classified into following:
| Virulence Factors | Characteristics |
| Help in attachment to host cell | |
| Microbial Surface Components Recognizing Adhesive Matrix molecules | Interact with host molecules like collagen, fibronectin and fibrinogen and facilitate cell attachment. Fibronectin binding proteins A and B, Collagen-binding protein, Staphylococcal protein A and clumping factor A and B are included in this family which are also involved in host immune invasion. |
| Break down of host immune shield | |
| Protein A | Binds to Fc portion of immunoglobulin, stop opsonization, works as super antigen and restricts the host immune response |
| Panton- Valentine Leukocidin (PVL) | Mostly found in community associated MRSA. It forms pores on cell membrane causing leakage of cell contents and finally death. |
| Polysaccharide microcapsule | combat phagocytosis by killing polumorphonuclear phagocyte. |
| Alpha toxin | First bacterial exotoxin to be identified as cell membrane pore former causing cell leakage and death |
| Chemotaxis-inhibitory protein | Extracellular protein that hinder chemotaxis functioning of neutrophil and monocytes. |
| Tissue Invasion | |
| Extracellular Adherence Protein | It is an exoprotein that binds with host plasma proteins, host cell matrix and endothelial cell adhesion molecule. It plays key role in adhesion, invasion as well as immune modulatory activity. |
| Proteases, nucleases, lipases, phospholipase C, metalloproteases, hyaluronatclyase and Staphylokinase | These are extracellular enzymes which are responsible for destruction of tissue thus helping in penetration of bacteria into tissues. |
| Induces Toxinosis | |
| Toxic Shock Syndrome Toxin -1 (TSST-1) | TSST-1 are known as pyrogenic toxin super antigens which is responsible for toxic shock syndrome in menstrual women. |
| Enterotoxins | S. aureus are responsible for production of varieties of enterotoxin that causes gastrointestinal infection. The Staphylococcal food poisoning is caused by the consumption of entertoxins contaminated foods and this is known as intoxication. |
| Exfoliative toxins A and B | It causes staphylococca-scalded skin syndrome especially in infants. |
Epidemiology and Transmission
About 20-30% human is persistently colonized by S. aureus. Intermittent colonization of S. aureus is found in an additional 30% of human population. Human anterior nares, oropharynx, axillae, groin and intestine are most often colonized by S. aureus. However some populations like health care workers, people with diabetes, hospitalized patients, people using drugs and immunocompromised individuals have higher rate of colonization. Subsequently, S. aureus colonization is a risk factor especially in immunocompromised people, people with chronic problems and surgical patients. Transmission is mainly by direct contact with people, animal and inanimate objects. S. aureus is responsible for about 25% of infection in hospitalized children among which 16% is caused by MSSA (methicillin sensitive S.aureus) and 9% by MRSA (methicillin resistant S. aureus). CDC report shows an annual incidence of severe infections more than 70,000 and 9000 death caused by MRSA. A significant difference is observed in rates of nasal carriage of S. aureus which reflects differences in healthcare, socioeconomics and occupational exposures according to global population studies.
Development in medicine such as transplantation, surgical procedures, implant devices, central venous catheter, dialysis and chemotherapy have shown significant increase in incidence and prevalence of S. aureus infection. Death due to bacterial bloodstream infections by S. aureus attribute to mortality of 30% in world. Due to this increase in infection by S. aureus, the burden on healthcare costs is increasing in today’s world.
S.aureus is transmitted through various routes:
- Most often spread by contaminated hands.
- Through breached skin, S. aureus enters to underlying tissues and cause infection.
- Person with immunocompromised or with invasive medical devices are especially vulnerable to S. aureus infection.
Clinical Manifestations
It varies according to the site of body where infection occurs. Staph infections occur commonly on skin which often looks like pimples. We might confuse with some kind of bite or ingrown hair.
Signs and symptoms of staph infection on skin include:
- Abscesses and boils: These are painful sores that form under your skin, causing pain and redness.
- Cellulitis: It causes red, swollen, painful skin and tissue just beneath skin.
- Folliculitis: These are small pimple-like blister under your hair follicle which causes pain.
- Impetigo: These are fluid-filled blisters or sores formed and ruptured leaving a yellow or brown crust.
- Staphylococcal scalded skin syndrome (SSSS): Causes skin to peel off all over the body and usually affects infants and small children.
These types of infection usually start in area which are tender, warm and red. As they get worse, they will form pus or drainage, with red areas getting bigger. Even some skin infections can become open wounds.
Signs and symptoms of staph infection on other part of body:
- Food Poisoning: Can be severe and include diarrhea and vomiting.
- Mastitis: Most commonly occurs in women who are breastfeeding, and leads to pain, inflammation and abscesses.
- Septicemia: When bacteria is in blood, it causes blood poisoning known as sepsis with symptoms like fever and low blood pressure.
- Toxic Shock Syndrome: It is the severe form of septicemia which includes fever, muscle aches and a rash that looks like sunburn.
- Endocarditis: Heart valves and heart muscles may be affected by staph and the symptoms are fever, sweating, weight loss and fast heart rate.
Laboratory Diagnosis
Sample Collection and Transportation
Depending on the site of infection, type of sample is determined.
| Infection | Specimen |
| Respiratory infection | Sputum |
| UTI | Mid Stream Urine |
| Suppurative Lesion | Pus, Wound swab |
| Bacteremia, PUO | Blood |
| Food Poisoning | Feces, Vomitus, food |
| Carriers | Nasal and perianal swab |
Direct Smear Microscopy
- Appear as GPC measuring 0.5-1.5 microns.
- Occur singly, in pairs, short chains or clusters.
- Present within and outside PMNs.
Gram Staining
- Appears as purple colored in grape like clusters, sometimes singly, in pair or in chain.
Culture
- Specimens are inoculated on the suitable media.
- Then the inoculated plates are incubated at 37˚C for about 24 hrs.
- On Nutrient Agar: colonies are golden yellow and opaque with smooth glistening surface, about 2-4mm in diameter, circular, convex and shiny.
- On Blood Agar: similar to that on nutrient agar, β-hemolytic.
- Liquid Medium: Uniform turbidity
- MacConkey Agar: small pink due to lactose fermentation
- Mannitol Salt Agar: Golden yellow colonies
Biochemicals Tests
- After culture, colonies from incubated plates are performed for biochemical tests and identified as S. aureus.
Treatments
Skin Infection:
- Treated with a topical antibiotic.
- May also drain a boil or abscess by making a small cut to pass the pus.
- Use of antibiotics depending on the type of infection. Choice of antibiotics for MSSA include Cephalexin, Dicloxacillin, Clindamycin, Amoxicillin etc. And for MRSA Cotrimoxazole, Clindamycin, Amoxicillin, tetracyclines, Doxycycline, Minocycline, Linozolid etc.
Lung Infections or pneumonia
- For MRSA Linezolid, Vancomycin, Clindamycin etc can be used.
Bacteremia or Blood Infection or infection from medical device
- The medical device needs to be removed first after the identification of infection. Then the antibiotics like Vancomycin, Linezolid, Nafcillin, Oxacillin, Cefazolin etc are used.
Endocarditis
- The foci is removed when possible and antibiotic such as Cefazolin, Gentamycin, Oxacillin, Nafcillin, Ciprofloxacin, Rifampin, Vancomycin, Daptomycin are used.
Meningitis
- For MRSA, Linezolid, Vancomycin, Clindamycin, Daptomycin, Cotrimoxazole etc are used.
- For MSSA, Oxacillin, Cefazolin, Nafcillin, Gentamycin etc are preferred.
Toxic Shock Syndrome
- Antibiotics such as Nafcillin, Clindamycin, Oxacillin etc are used for MSSA.
- For MRSA, antibiotics like Linezolid, Vancomycin, Clindamycin etc. are most commonly used.
Prevention and Control
- Practice and maintain good hand health.
- Appropriate use of antibiotics.
- Regular monitoring of air, water and surfaces to maintain proper environmental conditions.
- Proper disinfection of equipment and environments.
- Maintain proper hygienic conditions for medical procedures.
- Isolating patients when possible in clinical environments.
- Regular, proper and close monitoring of at-risk patients and people.
Antimicrobial Resistance
In 2019, S. aureus was the second leading pathogens responsible for death associated with antibiotic resistance. Resistance towards penicillin is due to penicillinase production (an enzyme which breaks the β-lactam ring of penicillin). Similarly, staphylococcal resistance to methicillin is via the mec operon which is a part of the staphylococcal cassette chromosome mec (SCCmec). mecA gene which codes for an altered penicillin binding protein is responsible for resistance in S. aureus and this is known as methicillin resistance S. aureus (MRSA). Aminoglycoside antibiotics like kanamycin, gentamycin, streptomycin which were once effective are now resistant towards S. aureus due to aminoglycoside modifying enzymes, active efflux of the drug out of bacteria and ribosomal mutation. Likewise, resistance to glycopeptide is mediated by acquisition of the vanA gene that originates from the Tn1546 transposon which is present in a plasmid of enterococci.
Conclusion
S. aureus is one of the important leading infectious agents responsible for morbidity and mortality worldwide. From mild skin infections to sepsis and pneumonia, these bacteria are responsible for causing varieties of illness. In recent year, development of antibiotic resistance had made it more difficult to treat infection by S. aureus and till date there is no vaccine available. The production of large numbers of toxins and presence of virulence factors and their effects are gaining a constant attention and a deeper understanding of their contribution will lead to the development of anti-virulence strategies.
References
- Nguyen Van An, A., Hai, L. H. L., Luong, V. H., Vinh, N. T. H., Pham, Q. H., Le, V. H., Nguyen, D. H., et al. (2024). Antimicrobial resistance patterns of Staphylococcus aureus isolated at a general hospital in Vietnam between 2014 and 2021. Infection and Drug Resistance, 17, 259–273. https://doi.org/10.2147/IDR.S437920
- Centers for Disease Control and Prevention. (2024, April 15). Staphylococcus aureus basics. U.S. Department of Health & Human Services.https://www.cdc.gov/staphylococcus-aureus/about/index.html
- Keim, K. C., & Herswill, A. R. (2023). Staphylococcus aureus. ScienceDirect , 31 (12), 1300-1301.
- Cleveland Clinic. (2022, June 7). Staph infection: Causes, symptoms, diagnosis & treatment. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21165-staph-infection-staphylococcus-infection
- Office of Research Safety, The George Washington University. (n.d.). Staphylococcus aureus (S. aureus). The George Washington University. https://researchsafety.gwu.edu/pathogen-data-sheets/staphylococcus-aureus-s-aureus
- Mandal, A. (2023, June 21). Staphylococcus Aureus Microbiology. News-Medical. Retrieved February 8, 2026, from https://www.news-medical.net/health/Staphylococcus-Aureus-Microbiology.aspx
- Aryal, S. (2024, December 19). Staphylococcus aureus – An overview. Microbe Notes. Retrieved February 8, 2026, from https://microbenotes.com/staphylococcus-aureus/
- Gnanamani, A., Hariharan, S., Paul-Satyaseela, M., & Ramesh, S. (2017). Staphylococcus aureus: Overview of bacteriology, clinical diseases, epidemiology, antibiotic resistance and therapeutic approach. In Frontiers in Staphylococcus aureus. IntechOpen. https://www.intechopen.com/chapters/54154
- Minnesota Department of Health. (2025, June 30). Staphylococcus aureus (S. aureus or “staph”) basics. Minnesota Department of Health. Retrieved February 8, 2026, from https://www.health.state.mn.us/diseases/staph/basics.html
- Acharya, T. (n.d.). Staphylococcus aureus: Disease, properties, pathogenesis and laboratory diagnosis. Microbe Online. Retrieved February 8, 2026, from https://microbeonline.com/staphylococcus-aureusdisease-properties-pathogenesis-and-laboratory-diagnosis/
- Mandal, A. (2023, June 21). Staphylococcus Aureus treatment. News-Medical. Retrieved February 8, 2026, from https://www.news-medical.net/health/Staphylococcus-Aureus-Treatment.aspx
- Cheung, G. Y. C., Bae, J. S., & Otto, M. (2021). Pathogenicity and virulence of Staphylococcus aureus. Virulence, 12(1), 547–569. https://doi.org/10.1080/21505594.2021.1878688
- Montero-Julian, F. (2020, March 2). Prevention and control of a Staphylococcus aureus infection. bioMérieux. https://www.biomerieux.com/corp/en/education/resource-hub/pharma-quality-control/scientific-library/prevention-and-control-of-a-staphylococcus-aureus-infection.html